Non-skeletal scoliosis describes nonstructurally-motivated spinal curvature and is usually a transient condition, although permanent cases can occur. A more common name for the condition is functional scoliosis. When the word functional is be added to many structural and/or back pain diagnoses, things get complicated. Diagnostic accuracy tends to plummet and lots of mistakes tend to be made during treatment protocols. Functional side-to-side spinal curvature is certainly no exception to this cruel rule.
Functional scoliosis is great, since it can often be corrected far easier than skeletal scoliosis in virtually all case profiles. In fact, many examples fully resolve all by themselves, often in less than a couple of weeks. Even when treatment is required, the interventions necessary will rarely involve surgery and certainly not spinal fusion, as is the only real curative option for skeletal scoliosis. However, not everything about functional scoliosis is positive either. The main problem lies in differentiating nonstructural cases of scoliosis from traditional spinal varieties.
This essay investigates the definition, causes and treatment of nonstructural scoliosis conditions. We will hope to prevent the common incidence of misdiagnosis in cases of functional scoliosis by propagating the truths of the condition for the benefit of patients and care providers alike.
What is Non-Skeletal Scoliosis?
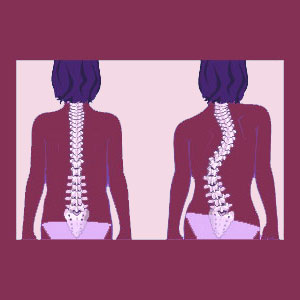
Functional scoliosis presents itself similarly to skeletal scoliosis. The spine will indeed feature one or more side-to-side bends and will often appear in every way to mimic normal scoliotic formation. However, the underlying cause is not related to any skeletal spinal issue. Instead, the entire symmetry and balance of the anatomy is being affected by some other root process that is also causing the spine to bend or twist similarly to traditional scoliosis.
In true scoliosis patients, there is some internal force inherent to the spine that is forcing it to curve. This force is considerable and can not be fixed by correcting posture, using exercises or performing stretches. In fact, this force is so great that even completely rigid back braces might have a difficult time keeping the curvature from worsening in select patient profiles. In functional scoliosis, this pressure within the spine is completely absent. Instead, the spine is being bent due to forces exerted from other structures in the body. In virtually all cases, these structures are muscular spasms, while in others, nonstructural versions of scoliosis might be caused by other skeletal abnormalities, often involving asymmetrical limb lengths.
Functional Scoliosis Causes
There are several common causations for functional scoliosis to occur, as well as some rare contributors. Below, we provide an overview of the most often seen causes of nonstructural spinal curvature:
Leg length differentials can unbalance the pelvis and cause one side of the body to tilt downwards or forwards. This change in normal posture and gait causes the spine to bend in response to the leg length difference in order to maintain proper alignment with gravity and upright function. Both structural and functional leg length differences can cause functional scoliosis and both can be easily corrected using appropriate therapeutic interventions in virtually all patients.
Similarly, sacroiliac joint dysfunction, imbalance and injury can offset the pelvis unilaterally, often causing minor causes of functional scoliosis.
Muscle spasms in the postural and dorsal musculature are the primary reason for most cases of functional scoliosis. The back muscles are extremely strong and can literally pull the spine out of normal alignment when muscles are locked in spasms or out of balance with their antagonistic pairings.
Treatment for Non-Skeletal Scoliosis
Proper treatment depends greatly on the underlying cause of nonstructural side-to-side spinal curvature. We detail the most effectual standards of care for each typical causation below:
Structural leg length differences can be easily resolved using orthotic inserts in shoes or specially-made orthotic shoes. Over a short span of time, the regular use of orthotics will allow the body to naturally rebalance itself, virtually eliminating all traces of scoliotic curvature. Functional leg length issues are rarely the cause of functional scoliosis, since they are usually incredibly subtle. For rare significant leg length differentials, exercises, stretches and manipulations can often bring the legs back into proper or relatively proper balance, reducing or resolving the functional spinal curvature consequence.
Sacroiliac joint concerns affecting anatomical symmetry might be easily treated with exercise, stretches and physical therapy when soft tissues are the cause. In cases of joint injury, sacroiliitis or congenital defect, the SIJ might benefit from fusion treatment, which is far less risky than spinal fusion. Either way, most SIJ contributors to functional scoliosis can be successfully eliminated.
Muscular spasms are certainly the main cause of clinical presentations of functional scoliosis. Spasms might occur for many reasons, including injury, degeneration, disease, infection, imbalances and mindbody causation enacted via ischemia. Therefore, treatment will vary greatly. Most cases will resolve by themselves, regardless of cause and will therefore only temporarily cause functional scoliosis. For chronic muscular spasms, treatment might be needed and can range from the use of physical therapy to correct imbalances and rehabilitate injury to the use of pharmacological treatment to calm spasms to the use of Botox to prevent any movement in the muscle to the application of knowledge therapy to get to the heart of mindbody pain conditions that are one of the most prevalent source of persistent muscle pain and spasms.
Scoliosis > Side to Side Spinal Curvature > Non-Skeletal Scoliosis